Last Updated:
Gastroparesis is not just “gas”, it is a real medical condition that deserves awareness, empathy, and proper treatment

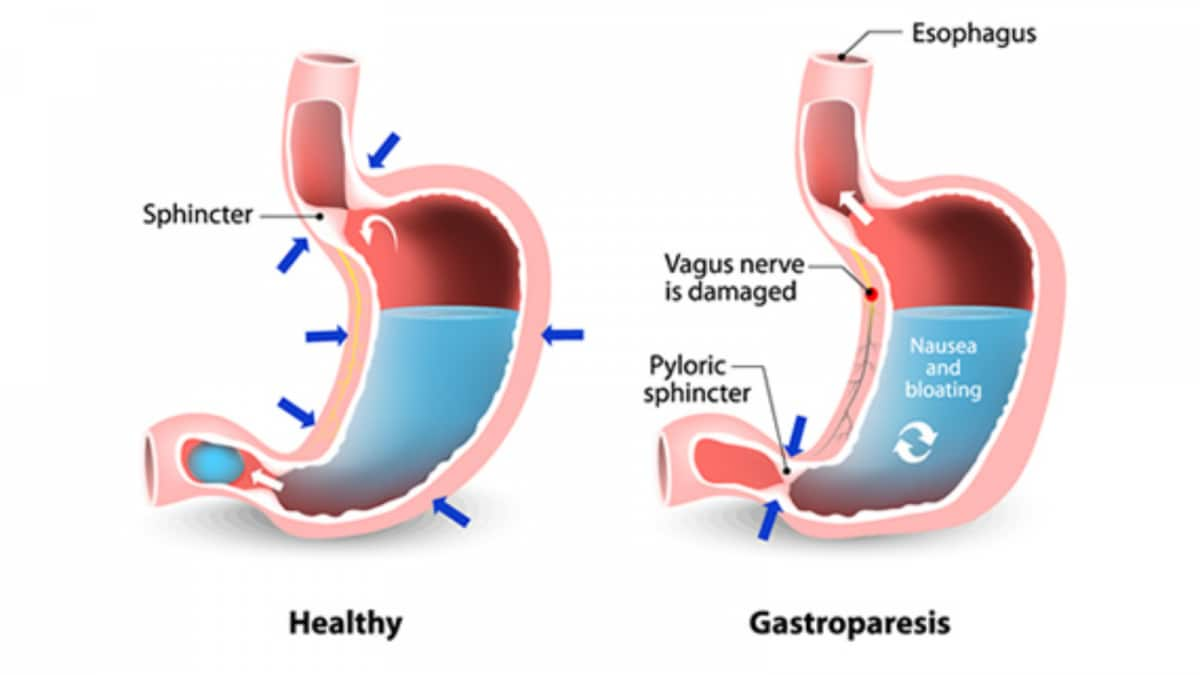
Gastroparesis is a chronic medical condition characterized by the stomach muscles not working well or at all, which delays the natural emptying of food into the small intestine
Gastroparesis, which is often misrepresented as a mild stomach complaint, is actually more akin to comparing a minor stomach problem like indigestion, acidity, or gas to a major storm. In reality, gastroparesis is a chronic medical condition characterized by the stomach muscles not working well or at all, which delays the natural emptying of food into the small intestine.
Patients’ experiences vary, but many report sensations of fullness or bloating, nausea, vomiting, abdominal pain, and difficulty finishing meals, often even difficulty eating at all. Sadly, because of persistent myths surrounding this condition, many people miss the chance to seek timely help and diagnosis that could improve their quality of life. Let’s break down the most common misconceptions. Dr. Ashok Kumar, Senior Consultant & Head, Gastroenterology, Sarvodaya Hospital, Greater Noida West shares all you need to know:
Myth 1: Gastroparesis is just gas or excess acidity
Fact: Gastroparesis is very different from the common indigestion we have all experienced. It is a serious condition involving abnormal stomach motility due to dysfunction of the nerves or muscles involved in digestion. Unlike acidity, symptoms do not resolve with simple antacids (e.g., Tums, Maalox).
Myth 2: Gastroparesis occurs only in older people
Fact: While more common in adults, younger patients can and do develop gastroparesis.
Myth 3: It is always due to poor eating habits
Fact: While diet plays a role in symptom management, gastroparesis usually results from damage to the vagus nerve (the nerve that stimulates stomach muscles). Causes can include diabetes, viral infections, or surgery not just dietary choices.
Myth 4: People with gastroparesis can’t eat anything
Fact: There is no lifetime food ban. With medical guidance, patients can manage symptoms by eating smaller meals and choosing low-fat, low-fiber foods. Nutrition tracking and mindful meal planning are crucial not starving.
Myth 5: There is no treatment
Fact: While gastroparesis may not completely resolve, there are several effective management options. Medications can stimulate stomach movement, dietary strategies can improve digestion, and in some cases surgical or device-based interventions are available. Many patients experience a significant improvement in quality of life.
Myth 6: It’s extremely rare
Fact: Gastroparesis is underdiagnosed, not rare. Many people with chronic nausea, bloating, or vomiting of unknown cause could actually have gastroparesis but are never evaluated for it.
Myth 7: Weight loss means the patient is improving
Fact: In gastroparesis, unintentional weight loss usually signals malnutrition and poor absorption, not recovery. That is the time to seek medical advice, not celebrate.
Myth 8: It’s just a stomach problem
Fact: Gastroparesis affects more than the stomach. It can cause dehydration, loss of electrolytes, and systemic health issues that impact overall wellbeing.
Takeaway
Gastroparesis is not just “gas”, it is a real medical condition that deserves awareness, empathy, and proper treatment. If you or someone you know experiences chronic bloating, nausea, or vomiting that does not respond to routine medications, it’s time to consult a gastroenterologist. Early diagnosis and treatment can truly change lives.

Swati Chaturvedi, a seasoned media and journalism aficionado with over 10 years of expertise, is not just a storyteller; she’s a weaver of wit and wisdom in the digital landscape. As a key figure in News18 Engl…Read More
Swati Chaturvedi, a seasoned media and journalism aficionado with over 10 years of expertise, is not just a storyteller; she’s a weaver of wit and wisdom in the digital landscape. As a key figure in News18 Engl… Read More